Subclause
6.4 – Disclosure of delays
ü
If an event
occurs in the PATIENT or the
equipment that should result in the generation of ALARM SIGNALS, the generation should occur promptly. For
example, clinicians would expect an ALARM
SIGNAL soon after an abrupt fall in heart rate to a
value below the lower ALARM LIMIT
for heart rate, or once apnea or asystole has
occurred. This is usually the case.
ü
However, in
some situations, ALARM
SIGNAL generation can be delayed to such an extent that
the delay can be clinically significant. This collateral standard recognizes
that there are two fundamentally different potential causes for these delays.
ü
First, it
can take some time for the ALARM
SYSTEM to determine that an ALARM CONDITION is present after the occurrence
of a valid triggering event in the PATIENT. This
delay is defined as the ALARM
CONDITION DELAY. It can be due to:
– artifact rejection algorithms, or
– INTELLIGENT
ALARM SYSTEMS that include event duration as part of the
algorithm, or
– aperiodic measurement (e.g., intermittent
non-invasive blood pressure monitoring).
ü
When the ALARM SYSTEM is aperiodically measuring rather than
continuously monitoring a variable, there can be a significant delay between
the time that an event occurs in the PATIENT and when
that event is detected. If the OPERATOR is unaware
of this, incorrect treatment decisions can occur. The time between measurements
is considered to be part of the ALARM
CONDITION DELAY.
ü
In the case
of apnea or asystole, the valid triggering event in the PATIENT has not occurred until the absence of
respiration or heart rate has existed for a defined period of time. Because
this defined period of time is required to pass before the event itself exists,
it is not included as part of the ALARM
CONDITION DELAY. See also the rationale for Definition 3.2.
M Second, the
generation of ALARM
SIGNALS can lag some time after the ALARM SYSTEM has determined that an ALARM CONDITION exists. This delay is defined in
this document as the ALARM
SIGNAL GENERATION DELAY. In most ALARM SYSTEMS this delay is usually clinically insignificant,
but can be important, for example, when paging systems or networked remote
devices are used to generate ALARM
SIGNALS. See also the rationale for Subclause 6.10.
אולי
ההנחיה צריכה
להיות
שההתרעות לא
תושהינה על
ידי רשת
התקשורת.
M A further
complication can occur when the ALARM SYSTEM is not continuously monitoring,
but is aperiodically measuring the variable that causes an ALARM CONDITION,
e.g. a non-invasive blood pressure monitor. There can be a significant delay
between when an event occurs in the PATIENT and when that event is detected. If
OPERATORS are unaware of this likelihood, incorrect treatment decisions can
occur.
זה
לא נכון להטיל
את האחריות על
המשתמש. הנכון
הוא לחייב זמן
השהיה מירבי
בשיעור של חלק
קטן 10-20% של הזמן
הנדרש לתחילת
הטיפול בחולה
ü
In that
case, the time between measurements is considered to be part of the ALARM CONDITION DELAY.
Figure A.1 illustrates the components of ALARM SYSTEM delay for a PHYSIOLOGICAL
ALARM CONDITION normalized variable.
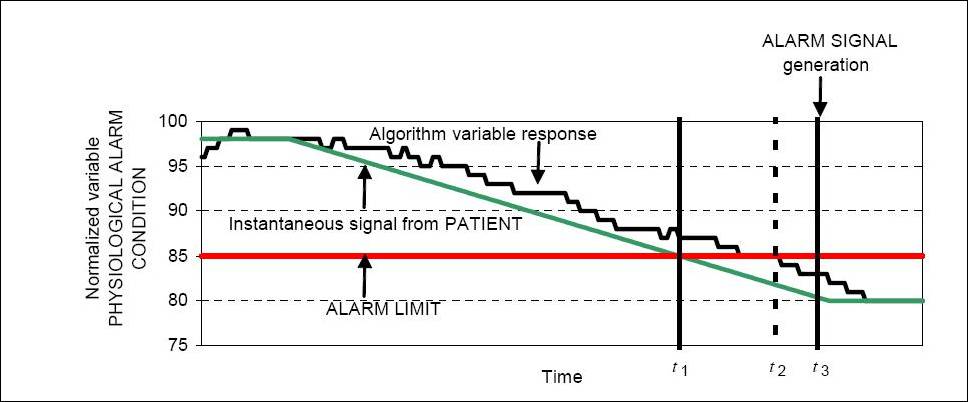
Figure
A.1 – Graphical representation of components of ALARM
SYSTEM delay
ü A valid triggering event occurs in the PATIENT at t1. At t2 the ALARM SYSTEM determines that an ALARM CONDITION exists.
û NOTE In this example, the ALARM LIMIT is less
than 85, not less than or equal to 85.
אין כמו הערה זו כדי להעיד על כך שסעיף זה של התקן זה כתוב במונחים מתמטיים-הנדסיים במקום במונחים של סיכון החולה.
The ALARM CONDITION DELAY is t2 – t1. This delay is due to the ALARM SYSTEM processing and
averaging.
The ALARM SIGNAL GENERATION DELAY is
t3 – t2. This delay is attributed
to the ALARM SYSTEM strategy
and the communication time to the ALARM
SYSTEM generating device or DISTRIBUTED ALARM SYSTEM (e.g. PATIENT monitor or central station).
At t3 the ALARM SYSTEM begins to generate ALARM SIGNALS.
Thus,
the overall ALARM
SYSTEM delay time is t3 – t1.